Once your cancer is diagnosed, your physician will determine the stage of the cancer. Melanoma is categorized into one of five main stages (0 through IV). The size, location and whether the melanoma has spread are used to determine the stage. Following your diagnosis, your doctor will use the staging information to select the best treatment options for you.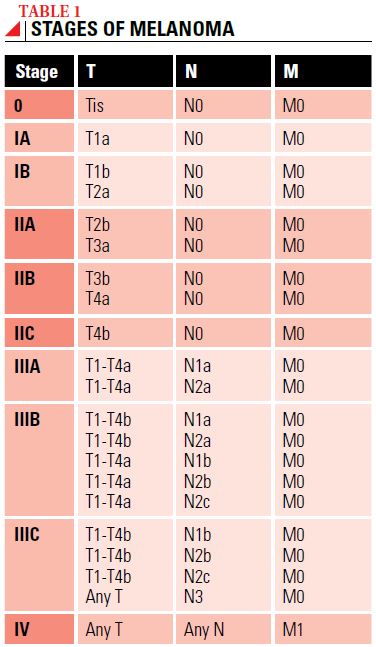

Melanoma is usually staged twice. First, your physician will consider the results of your physical exam and any imaging tests that were done, and assign a clinical stage. Then, after a biopsy or surgical procedure, a pathologist will examine tissue taken from the tumor (and possibly nearby lymph nodes) and assign a pathologic stage. Because the pathologic stage is based on more details about your specific melanoma, this second staging is more precise and is the key to deciding which treatment options may be best.
Both the clinical and pathologic stages of melanoma are classified according to the tumor, node, metastasis (TNM) system developed by the American Joint Committee on Cancer (AJCC) (see Table 2).
The first classification of the primary melanoma in the TNM system is for the thickness of the tumor (T). Each T classification is further divided into groups according to whether ulceration (a break in the outer layer of skin over the melanoma) is absent (subcategory a) or present (subcategory b).
For example, a non-ulcerated melanoma 3 millimeters (mm) thick is classified as T3a, whereas an ulcerated melanoma 2 mm thick is classified as T2b. Another factor for thin melanomas (less than 1 mm thick) is the mitotic rate, which measures how fast the cancer cells are dividing and multiplying.
The node (N) classification is used to describe how many lymph nodes contain melanoma cells. The N category includes subcategories to describe the number of cancer cells in the lymph nodes. If the cancer cells in the nodes can be seen only with a microscope, the metastasis (spread) is considered to be microscopic (a). If enough cancer cells are in the lymph node that the doctor can feel the mass during a physical exam or can see the mass on an X-ray, it’s said to be “macroscopic” lymph node involvement (b).
Another subcategory (c) indicates whether melanoma has spread to the lymphatic vessels leading to a lymph node. This is known as “in-transit melanoma,” which is metastatic melanoma found between the original tumor and the nearby cluster of lymph nodes.
The metastasis (M) category is used to classify the melanoma according to whether the cancer has spread beyond the region where the melanoma started to distant sites in the body.
Once the melanoma is classified according to the TNM system, an overall stage of disease is assigned (see Table 1). Stage 0 is known as “melanoma in situ” and is considered to be precancerous. Stage I and II melanomas are considered to be local (or localized) disease. Stage III melanoma is referred to as regional disease, and Stage IV is known as distant metastatic or advanced disease.

Words to Know
Biopsy – A procedure to remove tissue for examination to determine if melanoma is present.
Dermis – The dense inner layer of skin below the epidermis.
Epidermis – The upper layer of skin.
Lymph node – Found throughout the body, lymph nodes are small organs in the lymphatic system that filter lymph fluid, trapping bacteria, viruses and other foreign substances which are then destroyed by special white blood cells called lymphocytes. Cancer can spread to nearby lymph nodes.
Macrometastases – The spread (metastasis) of cancer from its original location to other sites in the body with the tumor large enough to be seen by the naked eye.
Micrometastases – The spread (metastasis) of cancer from its original location to other sites in the body with the newly formed tumors being too small to be detected by the naked eye. A microscope must be used.
Subcutaneous tissue – A deep layer of loose, irregular connective tissue beneath the skin.
©Patient Resource